What Is the Clotting Cascade?
The clotting cascade—also known as the coagulation cascade or secondary hemostasis—is part of the body's response to staunching bleeding after an injury. The word hemostasis is made up of "hem-" referring to blood, and -"stasis" which means "halt" in Ancient Greek.
Hemostasis is a potentially life-saving response to a bleeding injury. When the body can't respond quickly enough, for example when traumatic injuries occur, bleeding control products can help to accelerate the clotting process and potentially save the person’s life.
What Is the Clotting Cascade?
The clotting cascade is a series of processes that happen after bleeding caused by a tissue injury. This series of steps eventually leads to a blood clot which (ideally) stops the bleed. For clotting—or blood coagulation—to happen, coordinated actions are needed between the platelets and the coagulation factors.
The Four Stages of Hemostasis
The clotting cascade is one of the four stages of hemostasis. These are:
- The vessel spasm. The damaged blood vessel constricts to limit blood loss.
- Primary hemostasis (platelet clotting). During primary hemostasis, an unstable platelet plug is formed at the site of the injury.
- Secondary hemostasis (clotting cascade). During secondary hemostasis, the clotting factors activate to stabilize the plug. This staunches the blood flow, allowing more time for the body to repair any tissue damage.
- Fibrin clot remodeling. This provides a permanent solution to the problem. In this stage, the blood clot is remodeled into the same tissue the person had before sustaining an injury.
When the injury is small and these steps occur correctly, blood loss is minimized and the wound eventually heals. However, when somebody suffers a traumatic injury and loses a lot of blood, their blood becomes less able to clot. This means that they lose even more blood, and this can lead to mortality.
This problem—acute traumatic coagulopathy—as well as other serious conditions like shock can often be prevented by having a trauma kit on hand and knowing how to use it. If you or someone around you becomes injured and has moderate to severe bleeding, act immediately to stop the flow of blood.
Pathways in the Clotting Cascade
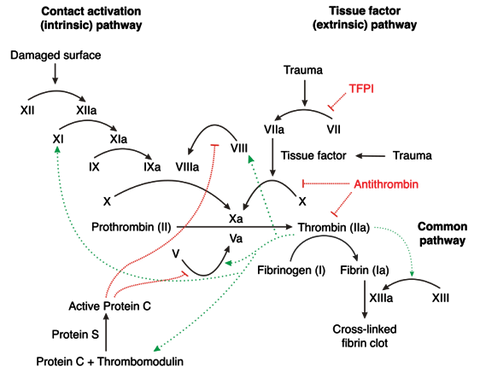
When an injury occurs, the clotting cascade (coagulation cascade) describes the process in which a series of clotting factors are activated one after another, ending in the fibrinogen-to-fibrin conversion that’s required to stabilize the blood clot that blocks the hole.
The clotting cascade can be categorized into three segments or pathways: the extrinsic, intrinsic, and common pathways. Factors found in the blood activate the intrinsic pathway whereas the extrinsic pathway is activated by tissue factors.
Extrinsic Pathway
The extrinsic coagulation pathway (starting on the outside of the skin) starts when tissue damage leads to tissue factor being exposed to the blood. Factor VII turns into Factor VIIa, which works with other factors to activate Factor X.
Intrinsic Pathway
The intrinsic coagulation pathway is longer than the extrinsic pathway and describes the process that occurs on the blood side (inside) of the wound. In this process, Factor XII becomes Factor XIIa after it's exposed to endothelial collagen. Similar transformations then happen:
- Factor XIIa causes Factor XI to turn into Factor XIa.
- Factor XIa then causes Factor IX to transform into Factor IXa.
- Factor IXa subsequently works with factors IIa and VIIIa to turn Factor X into Factor Xa.
This series of reactions is known as a cascade, as when a factor is activated, it activates more factors down the line. The concentration of factors increases as you get further down the cascade.
Common Pathway
Both the extrinsic and intrinsic pathways end up in the activation of Factor X, which leads to the common pathway involving Factor I, Factor II, and Factor V. The eventual transformation of Factor I (fibrinogen) into fibrin (Factor Ia) stabilizes the blood clot.
Coagulation Disorders
While most people's bodies will automatically stop blood leakage by forming blood clots, some people suffer from coagulation disorders that impede the formation of blood clots or cause the body to create them when they’re not needed. The inability to clot the blood makes sustaining an injury a lot more dangerous as the body is less able to stop the bleeding. If the body forms too many blood clots, there is an increased risk of blood vessel blockages.
A few of the most commonly known coagulation disorders are:
Hemophilia
Hemophilia is a genetic condition in which proper blood clotting doesn’t occur due to low levels of either Factor VIII or Factor IX. Hemophilia causes excessive bleeding, bruising, and swelling.
Von Willebrand Disease
This genetic disorder prevents proper clotting because the body doesn’t produce or utilize von Willebrand Factor normally. Von Willebrand Factor is a protein that helps to clot blood.
Venous Thromboembolism
Unlike the other two disorders, this condition causes the overproduction of blood clots. These clots form in veins. Parts of the clots can then break off and travel to the lungs, leading to a pulmonary embolism, which can be life-threatening.
Vitamin K-Dependent Factor Deficiencies
Some coagulation factors—II, VII, IX, and X, protein C, and protein S—are dependent on Vitamin K. A Vitamin K deficiency can lead to complications in blood clotting and even intracranial hemorrhage. Patients who are deficient in Vitamin K are generally treated with a high-dosage Vitamin K supplement.
How Do Doctors Diagnose Coagulation Disorders?
Coagulation testing can be performed to test how long clot formation takes and identify deficiencies in clotting factors.
- The PTT (partial thromboplastin time) test measures the protein factors in the intrinsic and common pathways: Factors XII, XI, IX, VIII, X, V, II, fibrinogen, prekallikrein (PK) and high molecular weight kininogen (HK).
- Another test, the PT (prothrombin time) test, measures the factors that are involved in the extrinsic and common pathways: Factors VII, X, V, II, and fibrinogen.
How Bleeding Control Products Assist With the Clotting Cascade
Bleeding control products such as hemostatic gauze contain hemostatic agents that help stop bleeding by sticking to the damaged tissues, concentrating clotting factors, and supplying procoagulant factors to the site of the hemorrhage. Hemostatic gauze is included in the premium version of our bleeding control kits.
Though bleeding control products are excellent tools for treating wounds, they can’t treat clotting disorders on their own. Patients with coagulation disorders may wish to keep bleeding control products on hand at all times while continuing treatment for their condition.
Bleeding Control Products Are Necessary for Serious Injuries
The body's natural response to bleeding is often enough to stem blood flow from everyday injuries. When small, non-serious accidents happen at work, at home, or when you're out and about, apply a Band-Aid and get on with your day.
However, being prepared for injuries that cause heavy bleeding can be the difference between life and death. Having a bleeding control kit with specialized items like hemostatic gauze close by can help you stop blood flow after an injury and potentially save your or someone else’s life.




